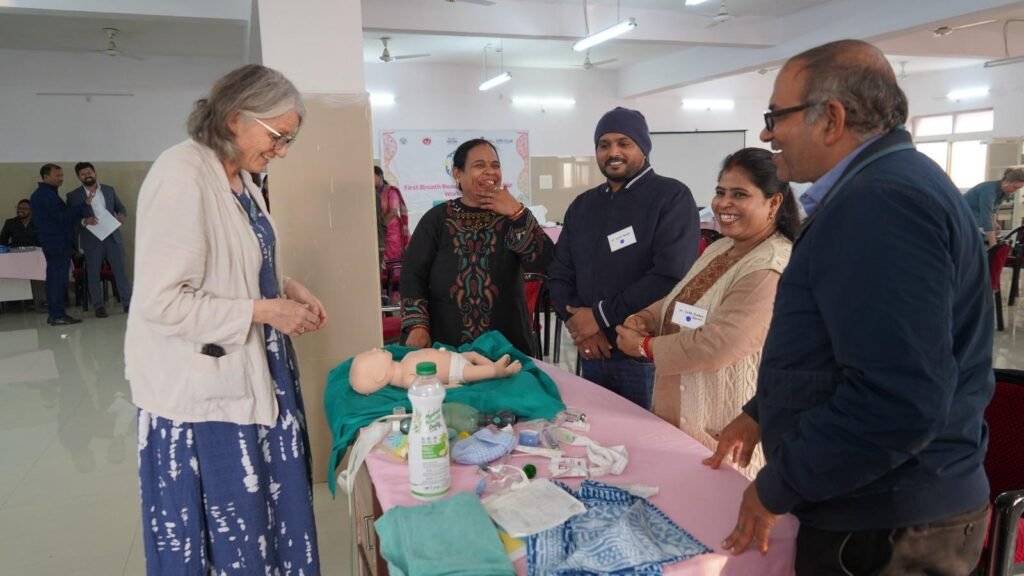
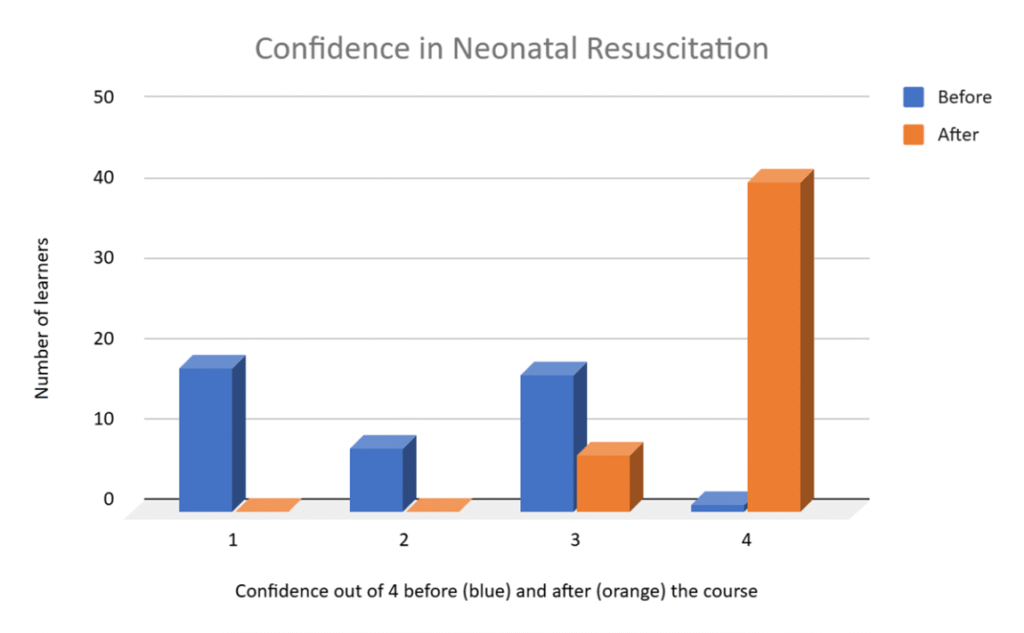
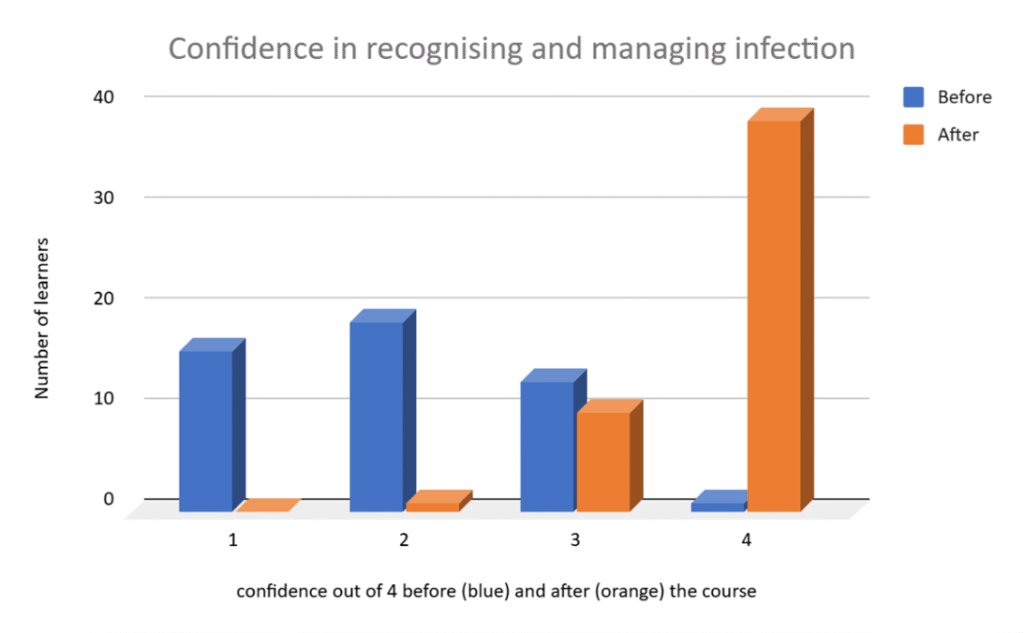
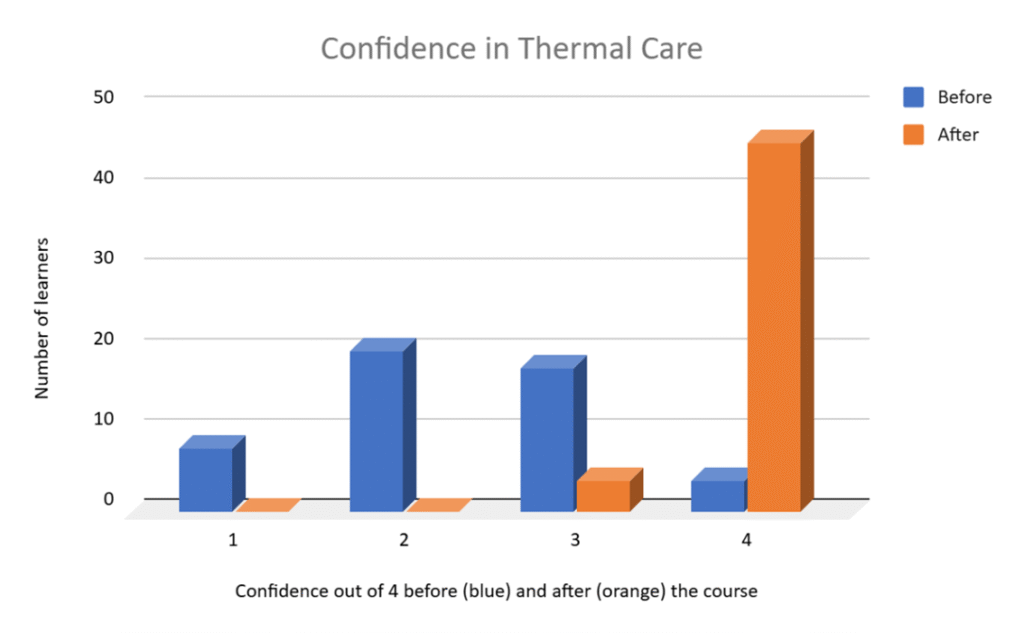
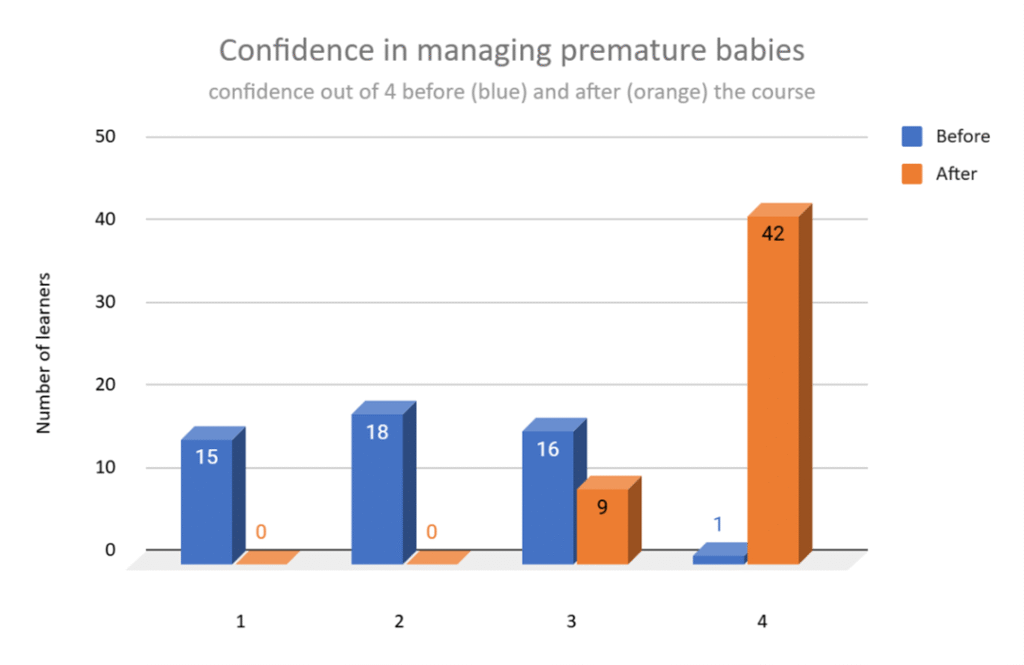
Feedback forms were received from 51 learners in all. 4 were nurses, 47 were medical officers (mainly doctors with an MBBS degree). Many of the medical officers had been qualified for over 10 years, one or two had been doctors for over 10 years but had only been caring for babies for the past 1 or 2 years. All 4 nurses are regularly working with birth attendants and attending deliveries. They were research nurses employed by CEL to support the birth attendants. They were not confident in resuscitation skills before the course but learnt quickly with the keenness of people who know they really need the skills. The increase in confidence levels is shown in the diagrams below. Confidence in all areas increased by the end of the course but there were more people scoring 3 out of 4 in all areas pre-course than we usually have, perhaps because of the overall higher level of training of these learners.
Free text feedback comments were all positive from the enjoyment of the course point of view and the perceived usefulness of the skills taught. Most of them had not been taught before using simulation techniques and this aspect of the course was much appreciated.
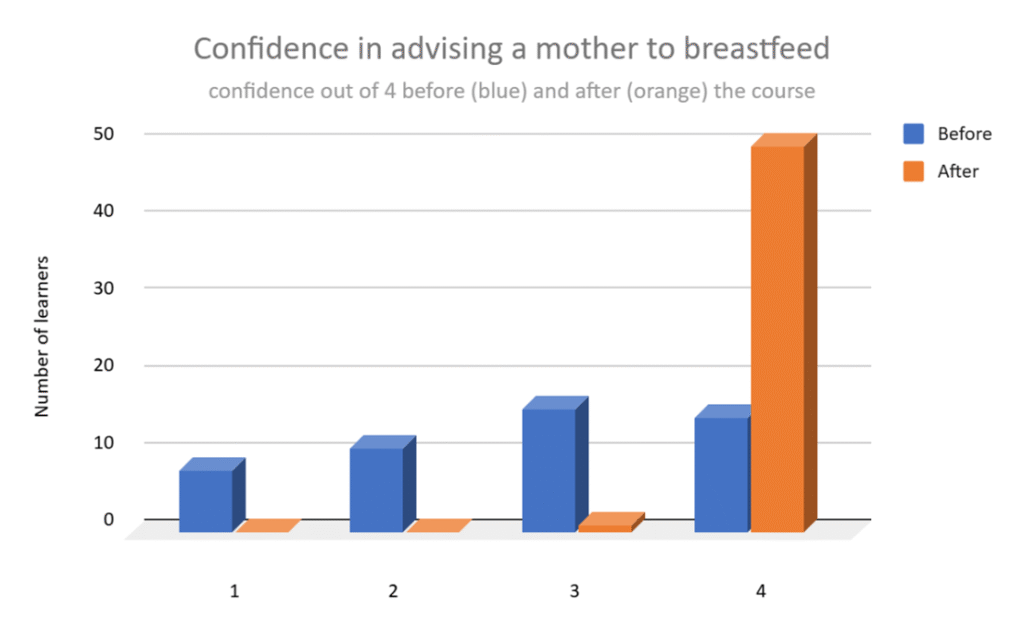
Interestingly, confidence in supporting a mother to breastfeed was quite high before the course but the questions on breastfeeding in the MCQ exam scored the lowest overall. This mismatch might be worth looking into – is breastfeeding generally thought of as a good thing but people are not so sure of how to help the mother with the practicalities of feeding?
A UNICEF report from 2024 states: breastfeeding is one of the most critical behaviours for child survival and growth. The NFHS-5 (2019-21) shows very low rates of early initiation of breastfeeding (EIBF) within an hour of birth for Uttar Pradesh at 24 per cent.
Key Breastfeeding Data (NFHS-5, 2019-21):
- Early Initiation (Within 1 Hour): Approximately 24% of infants.
- Exclusive Breastfeeding (0-6 Months): 41.5%.
- Prelacteal Feeding: Roughly 21% of infants receive prelacteal feeds (e.g., ghutti, honey)
- Colostrum Feeding: While many initiate feeding within 24 hours, about 15.4% of babies still do not receive colostrum.
Factors Affecting Rates:
Healthcare Practices: Lack of training for staff in some facilities hinders immediate, “skin-to-skin” contact.
C-Section Deliveries: A major factor causing delays in early initiation.
Social and Cultural Beliefs: Rituals such as delaying feeding until after a bath or discarding colostrum remain prevalent.