Undeterred, Judith found a microphone, the learners donned diocesan gowns from the vestry, moved their chairs to leeward and the lecture on the “Small Baby” continued.

Undeterred, Judith found a microphone, the learners donned diocesan gowns from the vestry, moved their chairs to leeward and the lecture on the “Small Baby” continued.

Two instructors and two learners on this second Neonatal Care Course have breastfeeding babies with them. Look at the size of them! Great to have real life role models; we should encourage this on UK courses.



23 countries, including Uganda, have achieved exclusive breastfeeding rates above 60 per cent. The other countries are Bolivia, Burundi, Cabo Verde, Cambodia, Democratic People’s Republic of Korea, Eritrea, Kenya, Kiribati, Lesotho, Malawi, Micronesia, Federated States of Nauru, Nepal, Peru, Rwanda, São Tome and Principe, Solomon Islands, Sri Lanka, Swaziland, Timor-Leste, Vanuatu, and Zambia. Is your country represented here? Can you do anything to get your own country on to this UNICEF list?
In Africa, nearly 70 per cent of countries have high rates of continued breastfeeding at one year, but in the Americas, only four countries have such high rates. [Source: https://www.unicef.org/uganda/press-releases/babies-and-mothers-worldwide-failed-lack-investment-breastfeeding]

Skills are taught as a 4-stage procedure – silent run through, demonstration with explanation, learners talking instructor through the skill and then all have a go. This imprints the skill on the learners’ minds. Which is why it is very important for the instructor to get it right and be consistent!

There is no piped oxygen in Bwindi Community Hospital. The grey machine on the floor here is an oxygen concentrator. If the ensuing oxygen/air mix is then piped through a bottle of mineral water, the pressure at which it reaches the baby’s nostrils can be increased. Preterm babies’ lungs tend to collapse with each expiration and putting them on this CPAP helps to prevent that.

We use the Global Health Media videos to illustrate much of what we are teaching. They are excellent videos on all aspects of medical care in resource poor areas of the world. Check out the breastfeeding ones which I think we should show more in the UK. Uganda has very high rates of breastfeeding so here we concentrate more on recognition of the sick infant, for which these videos are also very useful. https://globalhealthmedia.org/videos/
We’ve just finished Day 1 of the first Neonatal Care Course being taught by Ugandan instructors. All 12 instructors passed the Generic Instructor Course yesterday and rose to the challenge of teaching the NCC today. We are running this course in the chapel. Grace is course directing and made sure everyone knew the ground rules.

It wasn’t long before the newly trained instructors took over from us:



Dr Cath Harrison:
A visit to the paediatric ward today – an amazing set up with the ward being divided up into separate areas to allow patients needing frequent observations and management to be near the nursing station.
There is a kitchen at the end of the ward where families are taught by nursing staff the importance of nutrition and how to make nutritionally balanced meals.
There is an indoor play area and outdoor space as well for children.
We saw a variety of conditions – orbital cellulitis secondary to trauma (fall from a tree), pneumonia and malaria.
The pride was apparent in the quality of care the staff provided and the clinical space was so clean and tidy.
A good demonstration of teamworking to improve the quality of care provided to children and their families.

UK consultant neonatologist, Dr Cath Harrison, is part of the team in Bwindi this year and has written a couple of blog posts for the NICHE website:
During preparations for the GIC course, we were fortunate to have a visit to the Bwindi Community Hospital School of Nursing. This was set up in 2013 initially with 100 students. Now 10 years later there are 400 students. The course is 2-3 years long with students graduating with a Diploma in Nursing.
The school is about 3 minutes’ walk from the hospital entrance and is a self-contained facility with communal spaces, lecture theatres, library and on-site accommodation for the students. There is even a football pitch and the women’s team won a national competition last year!
The nursing school has improved nursing staffing for the hospital, with the best students being offered posts at BCH, thereby maintaining workforce and sustainable care provision.
There were 29 feedback forms from the first two NCCs in Uganda. All candidates were frontline healthcare workers and 25 (86%) of them had had previous experience of neonatal resuscitation.

Proving that neonatal mortality is falling as a result of our project is our long-term aim but measuring this outcome is a challenge. There are so many confounding factors in any clean data that is actually collected that it is almost impossible to prove that one intervention like this has any statistically significant effect on neonatal mortality.
It is more productive to measure shorter term outcomes which are known to correlate positively with an improvement in neonatal survival. We gather feedback from our learners on the usefulness of the course, their prior experience, suggestions for the future etc. but also on their increase in confidence levels in the practice of various skills taught on the course. The template for our feedback forms is based on one promoted by the UK’s Royal College of Paediatrics and Child Health for use on training courses.
Variations in self-confidence are known to influence motivation and tend to predict performance success. The percentage of learners in Bwindi in February feeling “very confident” in keeping babies warm increased from 17% to 100%, in giving breastfeeding advice, an increase from 24% to 100% post-course and in resuscitation skills, 7% to 93% feeling “very confident” after the course. Having the confidence to try and resuscitate an unconscious newborn baby is more likely to lead to a positive outcome than not having the confidence to make the attempt. Our data consistently show an increase in confidence in the essential skills pertaining to neonatal care identified by WHO. See: https://www.nicheinternational.org.uk/day-2-ncc-in-uganda/ for a screenshot of the questionnaires we use.


We are back in Entebbe now after 2 very successful Neonatal Care Courses, full of enthusiasm about returning in November to train the instructors we have identified.


Having 2 of the 4-member team nipping off to the neonatal unit in the middle of the day is not easy on the 2 left behind holding the baby – literally. Jarlath and Kirstie have been doing sterling work covering for our disappearing acts.



At one point, we came back to the lecture theatre to find that Jarlath’s lecture on convulsions had attracted a 16th learner.


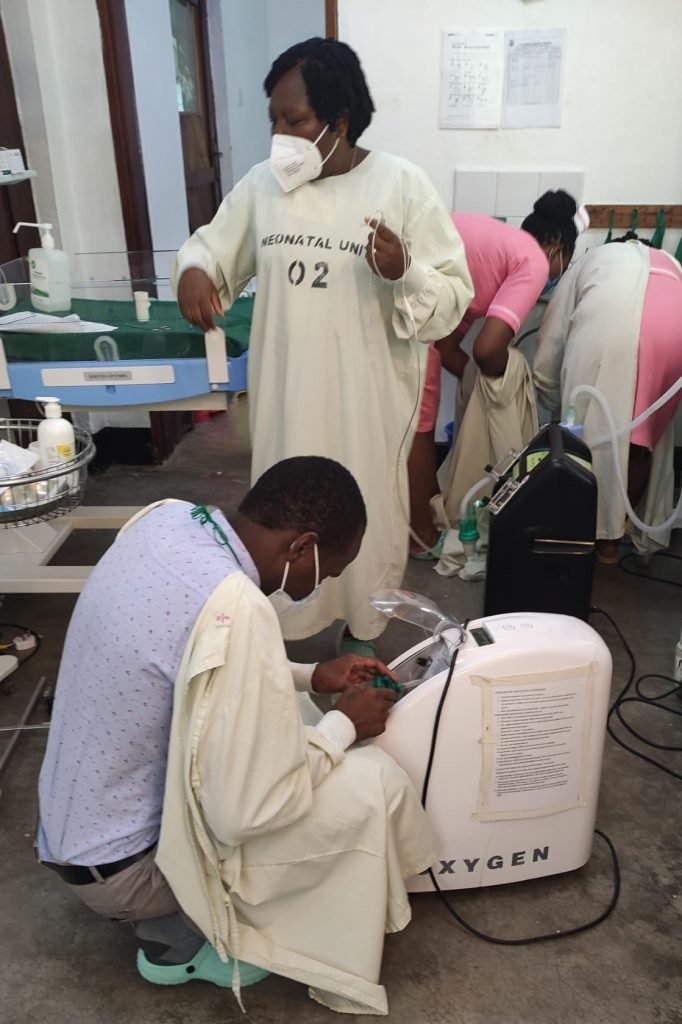
A premature baby (probably about 28 weeks gestation) was born on our first day in Bwindi. He weighed 1kg (2.2lbs). The paediatrician had just left the hospital and we were asked to help the young doctor pictured above who was covering the paediatric unit. Grace and Julia have visited daily for the last 5 days and supported the nurses in their excellent care of the tiny little boy who is now off CPAP and in skin to skin care with his mother for much of the day. It is normal for these babies to lose up to 10% of their birthweight and he now weighs 890g but is tolerating his expressed breast milk and I would expect him to start to put on weight from now on. He has had no blood tests, no x-rays and only homemade CPAP to support his breathing. He is a shining example of what good nursing care can do and we have used him throughout the course to illustrate what we teach about supporting preterm babies. These are the lives that can be saved by teaching staff the Neonatal Care Course.
